What test is utilized to evaluate superficial sensation? This question lies at the heart of this academic presentation, guiding us through a journey of exploration into the realm of sensory perception. Superficial sensations, encompassing touch, pressure, temperature, and pain, form the foundation of our interaction with the world, enabling us to perceive our surroundings and respond appropriately.
This presentation delves into the intricacies of superficial sensation, examining the tests employed to assess its function and the clinical significance of these evaluations.
Throughout history, the evaluation of superficial sensation has played a pivotal role in diagnosing neurological disorders and assessing sensory impairments. By understanding the principles and techniques involved in these tests, healthcare professionals can gain valuable insights into the integrity of sensory pathways and identify potential areas of dysfunction.
This knowledge empowers clinicians to make informed decisions regarding diagnosis, treatment, and rehabilitation strategies.
Definition of Superficial Sensation
/GettyImages-886098366-4d8b1aa36c0c465097651970685ca315.jpg)
Superficial sensations are sensations that arise from the skin and mucous membranes. They provide us with information about the external environment, such as touch, pressure, temperature, and pain. These sensations are essential for our everyday interactions with the world around us.
Physiological Mechanisms
Superficial sensations are mediated by specialized receptors located in the skin and mucous membranes. These receptors are activated by different types of stimuli, such as mechanical (touch and pressure), thermal (temperature), and chemical (pain). When a receptor is activated, it sends a signal to the spinal cord and brain, where the sensation is perceived.
– Describe the clinical significance of evaluating superficial sensation, including its role in assessing neurological function and sensory pathways.: What Test Is Utilized To Evaluate Superficial Sensation
Evaluating superficial sensation is crucial in assessing neurological function and sensory pathways. It provides valuable insights into the integrity of the peripheral and central nervous systems, helping clinicians diagnose and monitor neurological disorders and injuries.
Superficial sensation testing assesses the ability to perceive light touch, pinprick, and temperature changes on the skin’s surface. These sensations are mediated by specialized sensory receptors located in the skin and transmitted to the spinal cord and brain via sensory neurons.
By testing these sensations, clinicians can evaluate the function of these sensory pathways and identify any disruptions or abnormalities.
Types of Tests for Evaluating Superficial Sensation
Various tests are employed to assess superficial sensation, each utilizing specific stimuli, techniques, and equipment. These tests provide valuable insights into the integrity of sensory pathways and neurological function.
Light Touch Test
- Stimulus:A fine-tipped brush or cotton wisp
- Technique:Gently touch the skin at various points, asking the patient to indicate when they feel the touch
- Equipment:Brush or cotton wisp
Pinprick Test
- Stimulus:A sharp pin or needle
- Technique:Prick the skin lightly at various points, asking the patient to indicate when they feel the prick
- Equipment:Pin or needle
Temperature Sensation Test
- Stimulus:Cold and warm objects, such as a tuning fork or test tubes filled with different temperatures
- Technique:Touch the skin with the objects, asking the patient to identify the temperature as cold or warm
- Equipment:Tuning fork, test tubes
Two-Point Discrimination Test
- Stimulus:Two blunt probes or calipers
- Technique:Apply two probes to the skin simultaneously, varying the distance between them. Ask the patient to indicate when they feel two distinct points
- Equipment:Probes or calipers
Stereognosis Test
- Stimulus:Common objects of different shapes and textures
- Technique:Place the object in the patient’s hand, asking them to identify it by touch alone
- Equipment:Various objects (e.g., keys, coins, paper clips)
Light Touch Test

The light touch test is a neurological examination technique used to assess superficial sensation, specifically the ability to perceive light tactile stimuli. It is a simple and non-invasive test that can be performed in various clinical settings to evaluate nerve function and sensory pathways.
The light touch test involves gently touching the skin with a soft brush, cotton wisp, or monofilament at various points on the body. The patient is asked to indicate when they feel the touch. The examiner notes the presence or absence of sensation and any areas of decreased or absent sensation.
Significance of Light Touch Sensation
Light touch sensation is an important component of the sensory system, providing information about the environment and allowing for fine motor control. It is mediated by specialized nerve fibers called A-beta fibers, which are responsible for transmitting tactile and proprioceptive sensations.
Impaired light touch sensation can indicate damage to the peripheral nerves, spinal cord, or brain. It can be caused by various conditions, including peripheral neuropathy, spinal cord injuries, and neurological disorders.
Grading of Light Touch Sensation
The light touch test results are graded on a scale of 0 to 4:
- 0:No sensation
- 1:Decreased sensation
- 2:Normal sensation
- 3:Increased sensation
- 4:Painful sensation
Decreased or absent light touch sensation may indicate nerve damage, while increased or painful sensation may suggest nerve irritation or inflammation.
Procedure
To perform the light touch test, follow these steps:
- Explain the procedure to the patient and obtain consent.
- Position the patient comfortably and expose the area to be tested.
- Use a soft brush, cotton wisp, or monofilament to gently touch the skin at various points.
- Ask the patient to indicate when they feel the touch.
- Note the presence or absence of sensation and any areas of decreased or absent sensation.
- Repeat the test on the opposite side of the body for comparison.
Sample Report
The following is a sample report for documenting the results of the light touch test:
Light Touch Test:
- Right upper extremity: Normal sensation
- Left lower extremity: Decreased sensation in the distal toes
Limitations
The light touch test is a simple and useful screening tool, but it has some limitations:
- It is subjective and relies on the patient’s ability to report sensations accurately.
- It may not detect subtle changes in sensation.
- It can be affected by factors such as skin temperature and the patient’s level of alertness.
Alternative Methods
Alternative methods for assessing nerve function include:
- Pinprick test
- Temperature sensation test
- Vibration sensation test
- Two-point discrimination test
- Stereognosis test
These tests can provide a more comprehensive evaluation of sensory function and help identify specific nerve damage or neurological disorders.
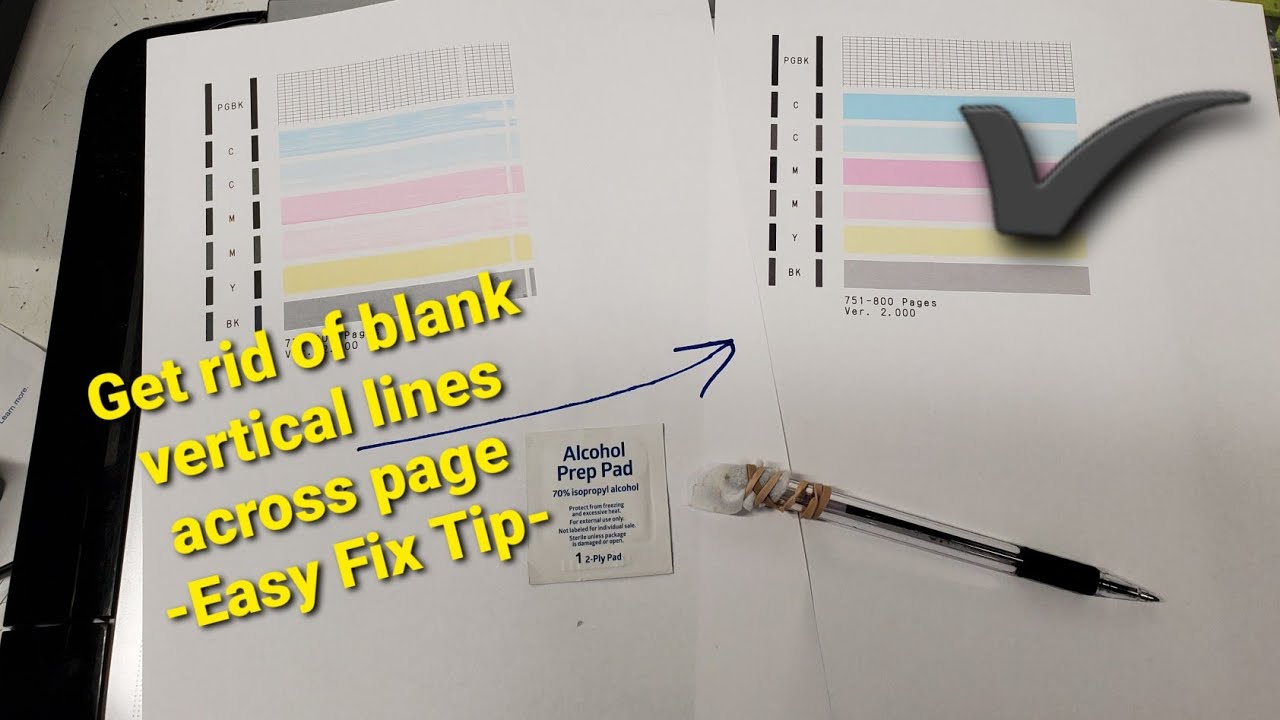
Pinprick Test
The pinprick test is a simple and non-invasive procedure used to evaluate pain perception and superficial sensation. It involves lightly pricking the skin with a sharp object, typically a sterile safety pin or a neurotip, to assess the individual’s ability to perceive sharp and dull stimuli.
The pinprick test is commonly used in neurological examinations to assess the integrity of the sensory pathways, particularly the spinothalamic tract, which transmits pain and temperature sensations from the periphery to the brain. It can help identify areas of sensory loss or impairment, which may indicate damage to the peripheral nerves, spinal cord, or brain.
Procedure
The pinprick test is performed by gently touching the skin with the tip of a sharp object, applying just enough pressure to indent the skin slightly. The patient is asked to report whether they feel a sharp or dull sensation.
The test is typically performed in a systematic manner, starting from the distal extremities and moving proximally towards the trunk.
Indications
The pinprick test is indicated in various clinical settings, including:
- Neurological examinations to assess sensory function and identify areas of sensory loss or impairment.
- Evaluation of peripheral nerve injuries or entrapment syndromes.
- Assessment of spinal cord injuries or lesions.
- Diagnosis of neurological disorders, such as multiple sclerosis or Guillain-Barre syndrome.
- Monitoring the progression or recovery of neurological conditions.
Limitations
The pinprick test has some limitations, including:
- Subjectivity: The test relies on the patient’s subjective report of their sensations, which can be influenced by factors such as pain tolerance, anxiety, or cultural differences.
- Accuracy: The accuracy of the test can be affected by the sharpness of the object used, the amount of pressure applied, and the patient’s cooperation.
- Incomplete assessment: The pinprick test only assesses pain perception and does not provide information about other sensory modalities, such as touch, temperature, or vibration.
Role in Evaluating Pain Perception
The pinprick test plays a crucial role in evaluating pain perception by assessing the patient’s ability to detect and differentiate between sharp and dull stimuli. It can help identify areas of sensory loss or impairment, which may indicate damage to the pain pathways or the perception of pain in the brain.
| Response | Interpretation |
|---|---|
| Sharp | Normal pain perception |
| Dull | Impaired pain perception |
| Absent | Severe impairment or loss of pain perception |
The results of the pinprick test can be interpreted using a flowchart to guide decision-making and further assessment. The flowchart typically involves assessing the patient’s response to the pinprick test and considering other clinical findings to determine the appropriate course of action.
Common Pitfalls
Some common pitfalls to avoid when performing the pinprick test include:
- Applying excessive pressure, which can cause discomfort or pain and affect the accuracy of the test.
- Using a dull or blunt object, which may not provide a sharp enough stimulus to elicit a response.
- Testing areas of the skin that are already numb or insensitive, as this will not provide meaningful information.
- Failing to consider the patient’s subjective report and relying solely on the objective findings.
Ethical Considerations
The pinprick test is generally considered a safe and ethical procedure. However, it is important to obtain informed consent from the patient before performing the test, especially if the patient has a history of pain sensitivity or anxiety.
Evidence Base
The pinprick test is a well-established and widely used method for evaluating pain perception and superficial sensation. Numerous studies have demonstrated its reliability and validity in assessing sensory function and identifying areas of sensory loss or impairment.
Future Research Directions
Future research directions for the pinprick test include:
- Developing standardized protocols to improve the accuracy and consistency of the test.
- Exploring the use of quantitative measures to objectively assess pain perception.
- Investigating the relationship between pinprick test results and other measures of sensory function, such as quantitative sensory testing.
- Examining the role of the pinprick test in monitoring the progression or recovery of neurological conditions.
Two-Point Discrimination Test
The two-point discrimination test is a neurological examination used to assess the ability of the sensory nervous system to distinguish between two distinct points of contact on the skin.
It is performed by gently touching the skin with two blunt probes, such as safety pins or calipers, at varying distances apart. The patient is asked to indicate whether they feel one or two points of contact.
Pinprick and light touch tests are commonly utilized to evaluate superficial sensation. These tests assess the patient’s ability to perceive sharp and dull stimuli applied to the skin. According to recent studies, the average cost of utility bills, including electricity, gas, and water, varies significantly depending on location and usage patterns.
Click here to learn more about average utility bills. Returning to the topic of superficial sensation, two-point discrimination testing is another method employed to determine the patient’s ability to distinguish between two distinct points of contact.
Clinical Significance
The two-point discrimination test is a valuable tool for evaluating the integrity of the sensory pathways, particularly the dorsal column-medial lemniscus pathway.
Impaired two-point discrimination can indicate damage to the peripheral nerves, spinal cord, or brain, and can be a sign of conditions such as diabetic neuropathy, multiple sclerosis, and spinal cord injuries.
The evaluation of superficial sensation, often utilizing the Semmes-Weinstein monofilament test, is crucial for assessing neurological function. Understanding what utilities are included in rent is equally important for individuals seeking housing. Essential services such as electricity, gas, and water are often included in rental agreements, while additional amenities like what utilities are included in rent may vary depending on the property and location.
These considerations impact the overall cost and comfort of a living space, just as superficial sensation testing provides valuable insights into sensory function.
Temperature Sensation Test
The temperature sensation test is used to assess the ability of the skin to detect changes in temperature. This test is performed by applying a warm or cold stimulus to the skin and asking the patient to identify the temperature.
The methods used to assess warm and cold sensations include:
Warm Sensation Test
The warm sensation test is performed by applying a warm stimulus to the skin, such as a warm water bottle or a heated probe. The patient is asked to identify the temperature as “warm” or “hot”.
Cold Sensation Test
The cold sensation test is performed by applying a cold stimulus to the skin, such as an ice pack or a cold water bottle. The patient is asked to identify the temperature as “cold” or “freezing”.
Clinical Implications of Temperature Sensation Abnormalities
Abnormalities in temperature sensation can indicate damage to the peripheral nerves or the central nervous system. For example, a loss of temperature sensation in the hands and feet can be a sign of peripheral neuropathy, while a loss of temperature sensation in the face can be a sign of a brainstem lesion.
Examples of Clinical Conditions that Can Cause Temperature Sensation Abnormalities
- Peripheral neuropathy
- Brainstem lesions
- Multiple sclerosis
- Guillain-Barré syndrome
- Diabetes
The following table summarizes the methods used to assess temperature sensation:
| Method | Description |
|---|---|
| Warm sensation test | Applying a warm stimulus to the skin and asking the patient to identify the temperature as “warm” or “hot”. |
| Cold sensation test | Applying a cold stimulus to the skin and asking the patient to identify the temperature as “cold” or “freezing”. |
The following flowchart Artikels the steps involved in interpreting the results of a temperature sensation test:
- Determine if the patient can identify the temperature of the stimulus.
- If the patient cannot identify the temperature, determine if the abnormality is unilateral or bilateral.
- If the abnormality is unilateral, consider a peripheral nerve lesion.
- If the abnormality is bilateral, consider a central nervous system lesion.
Case Study
A 50-year-old male presents with a complaint of numbness and tingling in his hands and feet. He has no other symptoms. On examination, he has a loss of temperature sensation in his hands and feet. The rest of his neurological examination is normal.
An MRI of the brain and spinal cord is unremarkable. The most likely diagnosis is peripheral neuropathy.
Stereognosis Test
The stereognosis test evaluates the ability to recognize objects by touch without visual input. It is a valuable tool in assessing tactile perception and object recognition, which are important aspects of neurological function.
During the test, the patient is blindfolded and asked to identify various objects placed in their hand. The objects may range from common items like keys or coins to more complex shapes like blocks or toys.
Role of Stereognosis in Tactile Perception and Object Recognition
Stereognosis relies on a complex interplay of sensory and cognitive processes. The tactile receptors in the skin transmit information about the object’s shape, texture, and temperature to the brain.
This information is then processed in various cortical areas, including the somatosensory cortex and the parietal lobe, which are responsible for integrating sensory input and forming a mental representation of the object.
The ability to recognize objects through stereognosis is essential for everyday activities such as manipulating tools, handling objects, and navigating the environment.
Graphesthesia Test
The graphesthesia test is a neurological exam used to assess the ability to recognize shapes and letters drawn on the skin. It is performed by lightly tracing a shape or letter onto the skin with a blunt object, such as a pen or key, and asking the patient to identify what was drawn.
Graphesthesia is a complex sensory function that involves the integration of multiple sensory modalities, including tactile sensation, proprioception, and kinesthesia. The ability to recognize shapes and letters drawn on the skin requires the patient to be able to feel the touch of the object, to sense the position of their body in space, and to move their fingers or toes in a coordinated manner.
Clinical Significance
The graphesthesia test is a valuable tool for assessing neurological function and sensory pathways. It can be used to detect damage to the peripheral nerves, spinal cord, or brain. Damage to any of these structures can disrupt the sensory pathways that are necessary for graphesthesia.
The graphesthesia test is also used to assess the recovery of sensory function after nerve injury or surgery. By comparing the patient’s performance on the graphesthesia test before and after surgery, the doctor can track the progress of the patient’s recovery.
Vibration Sense Test
The vibration sense test evaluates the ability to perceive vibrations, which are low-frequency mechanical oscillations. It involves applying a vibrating tuning fork to specific body parts and asking the patient to indicate when they feel the vibration.The vibration sense test is clinically significant because it assesses proprioception, which is the body’s ability to sense its position in space.
Proprioception is crucial for maintaining balance, coordination, and fine motor skills. Damage to the posterior columns of the spinal cord or peripheral nerves can impair vibration sense, leading to difficulty with balance and coordination.
Clinical Applications
The vibration sense test is used to diagnose various neurological conditions, including:
- Peripheral neuropathy (damage to peripheral nerves)
- Multiple sclerosis (an autoimmune disease that affects the central nervous system)
- Tabes dorsalis (a late complication of syphilis that affects the posterior columns of the spinal cord)
Reflexes
Reflexes are involuntary, stereotyped responses to specific stimuli that provide valuable information about the integrity of sensory pathways.
In the context of evaluating superficial sensation, reflexes play a crucial role in assessing the function of the dorsal column-medial lemniscus pathway, which is responsible for transmitting fine touch, proprioception, and two-point discrimination.
Types of Reflexes
The following are the main types of reflexes used to evaluate superficial sensation:
- Plantar reflex:Stroking the lateral aspect of the sole of the foot normally produces plantar flexion of the toes. An abnormal response, such as dorsiflexion (Babinski sign), may indicate damage to the corticospinal tract.
- Corneal reflex:Touching the cornea with a wisp of cotton normally elicits a rapid blink reflex. This reflex tests the integrity of the trigeminal nerve and its central connections.
- Cremasteric reflex:Stroking the medial aspect of the thigh in males normally produces contraction of the cremaster muscle, causing the ipsilateral testicle to elevate. This reflex tests the integrity of the genitofemoral nerve and its central connections.
- Anal reflex:Stroking the perianal skin normally produces contraction of the external anal sphincter. This reflex tests the integrity of the pudendal nerve and its central connections.
These reflexes, along with other sensory tests, provide a comprehensive evaluation of superficial sensation and help localize lesions within the sensory pathways.
Imaging Techniques
Imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, play a crucial role in evaluating superficial sensation by providing detailed anatomical visualizations of the sensory pathways and structures.
These techniques offer advantages in assessing sensory function by allowing clinicians to identify structural abnormalities, lesions, or other pathological conditions that may affect sensory processing.
MRI
MRI utilizes magnetic fields and radio waves to produce high-resolution images of the brain and spinal cord, enabling visualization of the sensory pathways and their connections.
MRI is particularly useful in detecting lesions, tumors, or other structural abnormalities that may disrupt sensory function, such as damage to the dorsal column-medial lemniscus pathway or the trigeminal nerve.
CT Scans
CT scans utilize X-rays to generate cross-sectional images of the body, providing detailed visualizations of bone structures and surrounding tissues.
CT scans can be used to identify fractures, dislocations, or other bony abnormalities that may affect superficial sensation, such as injuries to the peripheral nerves or nerve roots.
Specific Features
MRI and CT scans provide specific features that are useful for visualizing sensory structures:
- T2-weighted MRI:This sequence highlights fluid-filled structures, such as the cerebrospinal fluid surrounding the spinal cord and brain, making it useful for detecting lesions or abnormalities in these areas.
- Diffusion tensor imaging (DTI):This advanced MRI technique measures the diffusion of water molecules within tissues, providing insights into the integrity and connectivity of nerve fibers.
- Contrast-enhanced CT scans:Intravenous contrast agents can be used to enhance the visualization of blood vessels and other structures, aiding in the detection of vascular abnormalities or tumors.
Examples, What test is utilized to evaluate superficial sensation
Imaging techniques have been instrumental in identifying and characterizing sensory deficits in various clinical scenarios:
- Spinal cord injuries:MRI can reveal the extent and location of spinal cord damage, helping to assess sensory function and guide treatment decisions.
- Peripheral nerve injuries:CT scans can identify nerve root compression or other structural abnormalities that may be causing sensory deficits in the extremities.
- Multiple sclerosis:MRI can detect lesions and white matter abnormalities associated with multiple sclerosis, which can affect sensory function.
Future Developments
Ongoing research and technological advancements are continuously improving the capabilities of imaging techniques for evaluating superficial sensation:
- Advanced MRI techniques:Newer MRI sequences, such as functional MRI (fMRI) and magnetic resonance spectroscopy (MRS), are being explored to study the functional and metabolic aspects of sensory processing.
- Hybrid imaging:Combining MRI with other imaging modalities, such as positron emission tomography (PET) or single-photon emission computed tomography (SPECT), can provide complementary information about sensory function and metabolism.
Case Studies
Case studies provide valuable insights into the clinical applications of superficial sensation testing. By examining specific patient presentations, we can better understand the diagnostic and therapeutic implications of abnormal superficial sensation findings.
Superficial sensation testing is particularly useful in assessing neurological function and sensory pathways. Abnormal findings may indicate damage to peripheral nerves, spinal cord, or brain structures. Case studies can help us identify patterns of sensory loss or impairment, which can aid in localizing the site of the lesion.
Case Study 1: Diabetic Neuropathy
- Patient Presentation:A 55-year-old male with a history of diabetes presents with complaints of numbness and tingling in his feet.
- Superficial Sensation Testing:Light touch, pinprick, and temperature sensation tests reveal decreased sensation in the distal extremities.
- Results:The findings suggest peripheral neuropathy, a common complication of diabetes. The loss of superficial sensation indicates damage to the sensory nerves in the feet.
- Diagnostic and Therapeutic Implications:The diagnosis of diabetic neuropathy prompts further evaluation to assess the extent of nerve damage. Treatment focuses on managing blood sugar levels, preventing further nerve damage, and relieving symptoms.
Case Study 2: Spinal Cord Injury
- Patient Presentation:A 25-year-old female sustains a spinal cord injury at the C5 level following a motor vehicle accident.
- Superficial Sensation Testing:Light touch, pinprick, and two-point discrimination tests show impaired sensation below the level of injury.
- Results:The findings indicate damage to the ascending sensory pathways in the spinal cord. The loss of superficial sensation corresponds to the dermatomal distribution of the affected spinal segments.
- Diagnostic and Therapeutic Implications:The diagnosis of spinal cord injury guides further evaluation and treatment. Rehabilitation focuses on maximizing sensory function and promoting recovery.
Case Study 3: Stroke
- Patient Presentation:A 60-year-old male experiences a stroke involving the right hemisphere of the brain.
- Superficial Sensation Testing:Stereognosis and graphesthesia tests reveal impaired tactile perception on the left side of the body.
- Results:The findings suggest damage to the parietal lobe, which is responsible for processing tactile information. The loss of superficial sensation affects the patient’s ability to recognize objects by touch.
- Diagnostic and Therapeutic Implications:The diagnosis of stroke prompts immediate medical intervention. Rehabilitation focuses on improving sensory function and re-establishing neural connections.
FAQs
What is the purpose of evaluating superficial sensation?
Evaluating superficial sensation helps healthcare professionals assess the function of sensory pathways and identify potential neurological disorders or impairments.
What are the different types of tests used to evaluate superficial sensation?
Common tests include light touch, pinprick, temperature sensation, and vibration sense testing.
What is the clinical significance of abnormal superficial sensation findings?
Abnormal superficial sensation findings may indicate damage to sensory pathways or neurological structures, suggesting the presence of underlying neurological disorders.